In December 2020, amid a renewed surge of SARS-CoV-2 cases that saw COVID-19 pandemic deaths top more than 1.6 million people worldwide,1 we heard the news we had been waiting for: a vaccine had finally been approved. Pfizer, in partnership with BioNTech, was the first to receive Emergency Use Authorization (EUA) from the FDA.2 That same month, Moderna’s vaccine was also granted EUA.3
The two vaccines share quite a bit in common: they both smashed records for vaccine development speed. They are both highly effective.4,5 They are both RNA vaccines. And they are the first of their kind to receive emergency authorization from the FDA.
A new breed of vaccine
Unlike traditional vaccines, which typically use either weakened or inactivated virus to induce immune responses, RNA vaccines use messenger RNA (mRNA) that delivers instructions to our cells. The mRNA teaches our cells how to make a viral protein (in this case, the SARS-CoV-2 spike protein) that can then be identified by our immune system. Though this technology offers a number of advantages, including eliminating the use of potentially infectious elements and a shorter development time, it also presents some hurdles.
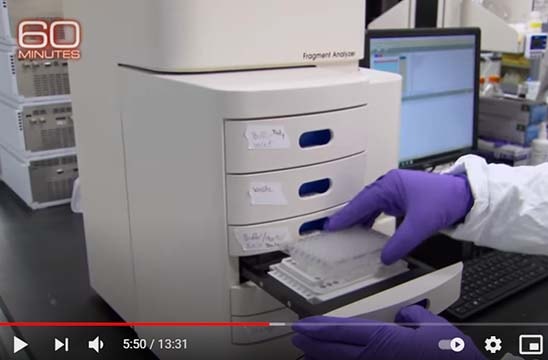
While these RNA vaccines represented a promising technology, no RNA vaccine had been approved by the FDA. Another challenge was the use of RNA: as RNA is unstable and degrades easily, these vaccines require stringent quality control (QC) protocols and sensitive tools to ensure RNA integrity and quality. One such tool is the Agilent Fragment Analyzer system, which uses automated parallel capillary electrophoresis to provide reliable QC. The ability to evaluate more RNA samples in less time, with less effort by researchers has become crucial—hundreds of laboratories worldwide have adopted the Fragment Analyzer automated capillary electrophoresis systems to help transform their total RNA analysis with speed, accuracy, and automation. Our Fragment Analyzer system can be seen in a recent 60 Minutes segment titled, “How the Pfizer-BioNTech COVID-19 vaccine was developed.”
Exceeding expectations
In spite of the difficulties facing them, Pfizer, BioNTech, and Moderna rose to the challenge. Historically, vaccines have taken 5–10 years to develop, with the mumps vaccine—taking only 4 years—being a speedy outlier.6 In February 2020, the World Health Organization made what was considered to be an optimistic projection by saying a SARS-CoV-2 vaccine could be ready in 18 months.7 And, ten months later, the Moderna and Pfizer vaccines exceeded expectations by receiving EUA approval.
These vaccines also outperformed when it came to effectiveness. In their initial guidelines8 for industry vaccine development, the FDA stated, “…the primary efficacy endpoint estimate for a placebo-controlled efficacy trial should be at least 50%....” For perspective, the yearly influenza vaccine has an average efficacy between 40 and 60%;9 both the Moderna and Pfizer vaccines shattered these endpoint goals with, respectively, 94 and 94.8% efficacy.4,5
Reshaping the pandemic
With vaccines now available, immunization campaigns are underway in many countries. While logistical and vaccine supply challenges remain, at the time of writing more than 189 million vaccine doses have been administered in the United States alone10—and the pace is accelerating. At the forefront of vaccinations is Israel where, as of April 13th, 2021, 57.31 and 53.23% of the population has received their first and second doses, respectively.
The ultimate aim of these vaccination campaigns is to provide herd immunity, where a large enough proportion of a population has gained immunity that it lessens the risk of transmission to people without immunity. Unfortunately, the threshold to achieve herd immunity against SARS-CoV-2 remains unclear and will likely depend on a number of vaccine and community-dependent factors.11 It is likely, however, that achieving herd immunity will require the vaccination of not just adults but children as well, which is why both Pfizer and Moderna have begun clinical trials for children 12 years of age and older.12,13
Conclusions and retrospectives
It is something of an understatement to describe the past year as "challenging." The COVID-19 pandemic has been a constant source of uncertainty and fear for everything from personal health to supply chain breakdowns. Some were unable to gather with family for the holidays. Some will never be able to gather again. But if there are positives to be taken from this pandemic, they are that we are more resilient than we thought. And we are stronger than we thought.
In a recent interview, Dr. Albert Bourla, CEO of Pfizer, stated, “I believe in the power of science. I believe in the miracles that science in the private sector can do for mankind.” For anyone who has worked in a lab, taking a therapeutic from concept to clinic in barely a year would easily qualify as such a miracle—and yet it was done not once, but twice.
The vaccine, unfortunately, is not an immediate solution for the pandemic. Our work is not done, as we all need to continue working together and minimizing the spread until herd immunity has been established. But, for the first time, we now have the tools to begin forging a path out of the COVID-19 pandemic.
References:
- Weekly epidemiological update - 22 December 2020 https://www.who.int/publications/m/item/weekly-epidemiological-update---22-december-2020 (accessed Feb 23, 2021).
- Office of the Commissioner. Pfizer-BioNTech COVID-19 Vaccine https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/pfizer-biontech-covid-19-vaccine (accessed Feb 23, 2021).
- Office of the Commissioner. Moderna COVID-19 Vaccine https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/moderna-covid-19-vaccine (accessed Feb 23, 2021).
- Polack, F. P. et al.; C4591001 Clinical Trial Group. Safety and Efficacy of the BNT162b2 MRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383 (27), 2603–2615.
- Baden, L. R. et al.; COVE Study Group. Efficacy and Safety of the MRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384 (5), 403–416.
- Young, M. L. et al.: Experiences with Jeryl Lynn Strain Live Attenuated Mumps Virus Vaccine in a Pediatric Outpatient Clinic. Pediatrics 1967, 40 (5), 798–803.
- WHO Director-General’s remarks at the media briefing on 2019-nCoV on 11 February 2020 https://www.who.int/director-general/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 (accessed Apr 13, 2021).
- Center for Biologics Evaluation; Research. Development and Licensure of Vaccines to Prevent COVID-19 https://www.fda.gov/regulatory-information/search-fda-guidance-documents/development-and-licensure-vaccines-prevent-covid-19 (accessed Feb 23, 2021).
- Vaccine effectiveness: How well do the flu vaccines work? https://www.cdc.gov/flu/vaccines-work/vaccineeffect.htm (accessed Apr 13, 2021).
- CDC. COVID Data Tracker https://covid.cdc.gov/covid-data-tracker/ (accessed Apr 13, 2021).
- Coronavirus disease (COVID-19): Herd immunity, lockdowns and COVID-19 https://www.who.int/news-room/q-a-detail/herd-immunity-lockdowns-and-covid-19 (accessed Apr 13, 2021).
- Study to Describe the Safety, Tolerability, Immunogenicity, and Efficacy of RNA Vaccine Candidates Against COVID-19 in Healthy Individuals https://clinicaltrials.gov/ct2/show/NCT04368728 (accessed Feb 23, 2021).
- A Study to Evaluate the Safety, Reactogenicity, and Effectiveness of mRNA-1273 Vaccine in Adolescents 12 to <18 Years Old to Prevent COVID-19 https://clinicaltrials.gov/ct2/show/NCT04649151 (accessed Feb 23, 2021).